Combatting the crown: Strategies for coronavirus vaccines
Review
Subhajit Bandyopadhyay

Our fight against the COVID19 pandemic began simultaneously with it's onset. While earlier strategies were curative in nature, research has now moved on to preventive measures and multiple vaccines are being developed across the globe. This article discusses the science behind these vaccines and how they function.
Tweet
The better part of 2020 was painful - involving home isolations, resulting in a lack of social interactions and tremendous anxiety due to the ongoing state of affairs. For scientists, the year was additionally challenging, for they required to meet societal expectations by rising to the occasion of the pandemic and delivering its remedies. They worked hard, in fact, very hard, with one goal - to release mankind from the grip of the evil virus by delivering vaccines that work. As proud citizens of the world’s largest vaccine-producing country[1], it is a natural curiosity of the people to know the key strategies employed to develop the COVID-19 vaccines.
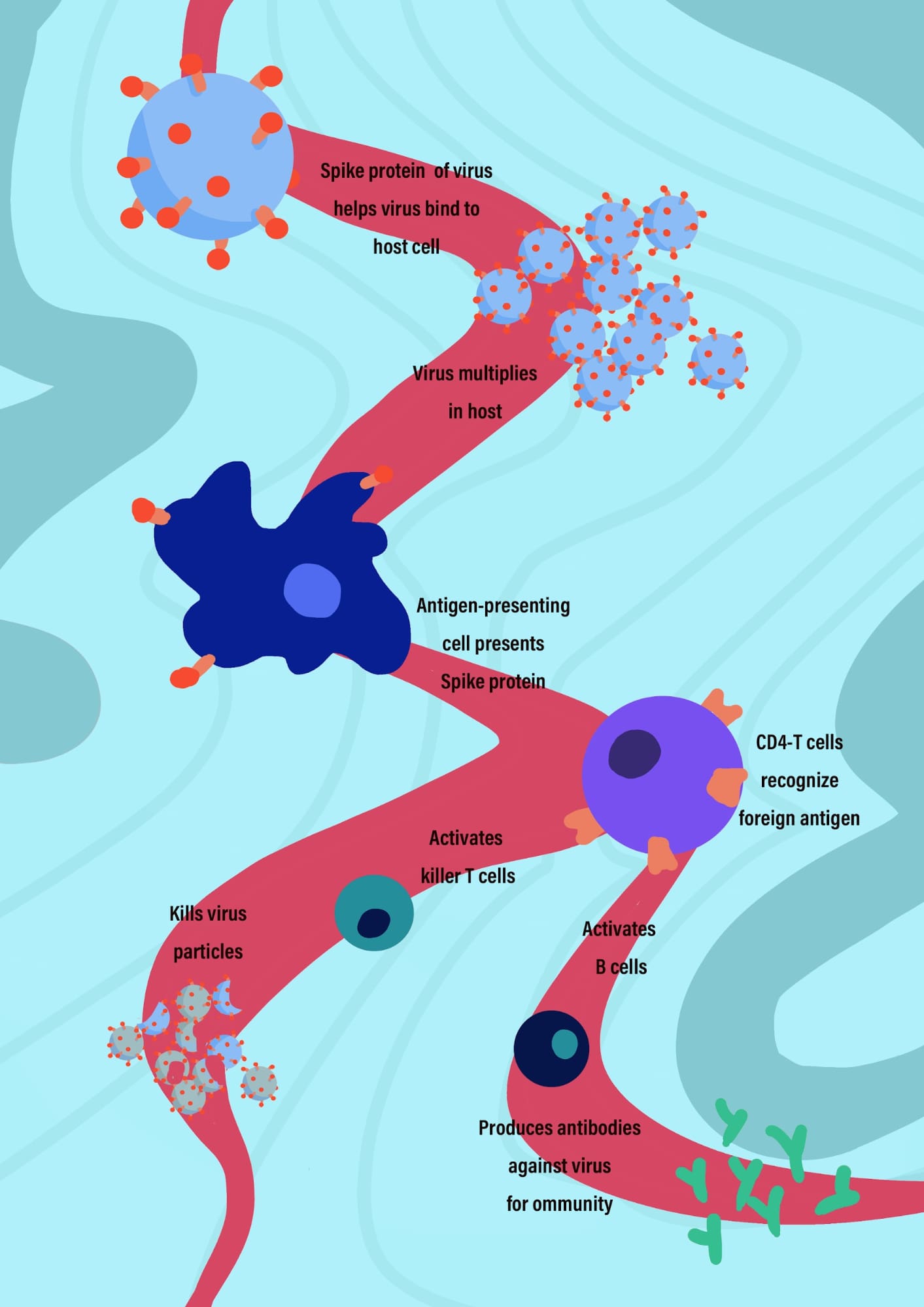 Immune response
Immune response
Credits- Vadlamannati Vijaya Arunima
It is important that we quickly refresh our memory on the enemy, the novel coronavirus. As you must have seen a zillion times by now in all sorts of news resources and the media, the structure of the coronavirus is like a puffed pufferfish, a ball-like creature with spikes all around.
The spikes that are around the coronavirus are called the S-protein. If you try to grab a pufferfish, you touch the spikey surface first. Similarly, when the coronavirus comes in contact with a surface (for example, our body), it lands on its spikes. Therefore, the spikes of the virus consisting of the S-protein (S, as you might have guessed, stands for spike) is the key component for the attachment of this virus to a cell prior to launching its invasion. Therefore, to beat the coronavirus, these S-proteins need to be dealt with. Note that this S-protein in itself is harmless, like the legs without a body[2].
What do we do if we want to stop you from running around? We can put a sack around your legs, and that impedes your mobility. The approach to the vaccine design is quite similar. We need to make the sacks (also proteins) against the Spike-protein[3].
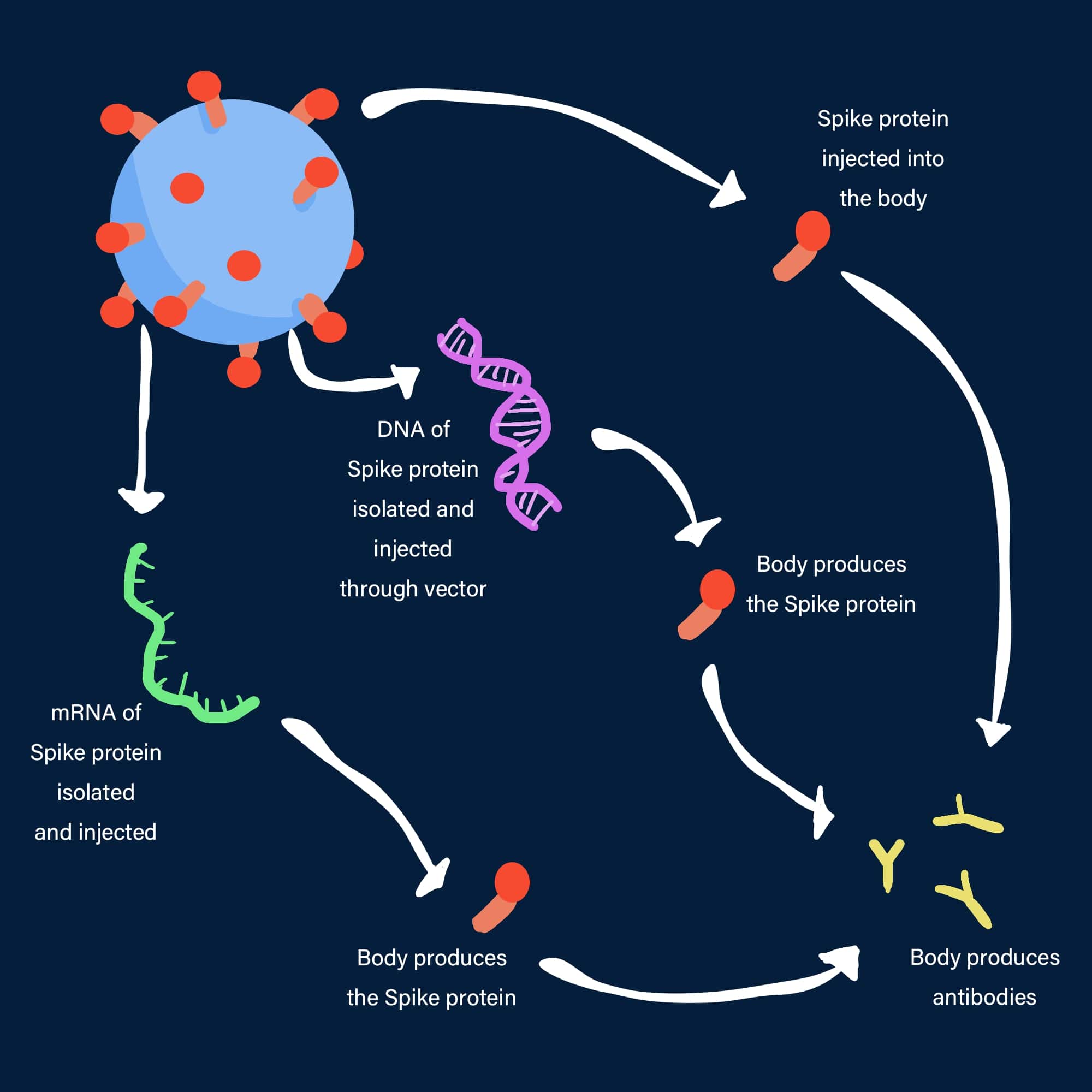
There are three different approaches to deactivate these S-proteins. It would require an introduction to some technical terms. I will do so as I proceed.
The first registered vaccine for COVID-19 that came into use is the Russian Sputnik V vaccine. It relies on an age-old piggy-back mechanism involving another virus that is known to our body such as the virus for the common cold (technically called adenoviruses). They are a class of less harmful viruses. The gene from the coronavirus that makes the S-protein is inserted into the adenovirus. Then the adenovirus is deactivated so that it cannot multiply inside our body, and thus rendered harmless. The adenovirus, when injected acts as the delivery van that delivers the S-protein expressing gene into our body. This starts the production of just the S-protein inside us, which itself is not harmful. What can the legs (S-proteins) do alone without the body (the whole virus)? However, our immune system still recognizes this as a foreign object and produces antibodies against it. The antibody is like the sack to put around the legs – the analogy that I gave earlier. Now the body is immune and ready to deal with the real coronavirus. When the real coronavirus attacks us, the immune system of our body is now trained to neutralize the S-proteins that are present on the surface of the virus. Thus, the dangerous virus cannot attach itself to our cells and cannot multiply without “feeding on” our cells[4].
 The three strategies for COVID-19 vaccine
The three strategies for COVID-19 vaccine
Credits - Vadlamannati Vijaya Arunima
The Russian vaccine requires a second booster dose after three weeks. This booster dose uses a second delivery van (adenovirus) as the delivery vehicle. This reinforces our immune system exactly in the same way it did earlier. It was found that using two different delivery vans makes the memory of our immune system better. So, our body remembers how to deal with these S-proteins or S-protein-decorated coronavirus for a longer time, providing a long-term immunity.[5].
The Oxford-AstraZeneca vaccine is also a forerunner in vaccine development that uses the genetic material that can code for the S-protein and is put inside an adenovirus (a cold virus from a chimpanzee). These systems are cheaper than some of the other vaccines and do not require a very low temperature to store them[6].
Then there is the Pfizer vaccine that made the headlines in a big way. The Pfizer vaccine is an mRNA vaccine[7]. The messenger RNA (mRNA in short) is an RNA that carries the information for synthesizing a protein in the ribosome of a cell. An mRNA of the virus codes for a protein of the virus and uses the victim’s cells and its components to prepare the protein. Now, when the mRNA that codes for the S-protein is injected into our body, it instructs our body to produce the harmless S-protein. The S-protein is produced in the body and expressed on certain cell surfaces. Although they are harmless, our immune system sees them as foreign objects on the cells and stimulates an immune response. Antibodies are generated against it to neutralize it. The RNAs are single-stranded (unlike the double-stranded DNA) and not very stable molecules. They breakdown by themselves if left in vials at room temperature for a very long time. They can be preserved at a very low temperature, such as -70 °C. That is why several governments were concerned about the delivery of mRNA vaccines to remote clinics, where such low-temperature storage systems are not available. American biotechnology and pharmaceutical company Moderna also takes a similar approach. Moderna’s vaccine, working on the same principle, is stabilized by a polymer and preserved at a higher temperature[8].
The third approach uses the S-protein that is produced in the lab using recombinant technology- a state-of-the-art biotech tool. The S-protein is delivered into our bodies and triggers an immune response to generate the antibody that neutralizes the S-protein. The Novavax and Sanofi-GlaxoSmithKline vaccines are such protein-based vaccines[9]. The Novavax vaccine is interesting as it is a 3D assembly of several S-proteins which mimics the shape and the size of the actual virus[10]. This assembly itself is harmless yet it generates an immune response and produces the antibody that protects us from the actual virus.
To date when this article has been written, it is now known to all that two vaccines have been approved for the Indian population. A third might be underway. The first one, Covishield, is the Oxford-AstraZeneca vaccine produced by the Pune-based Serum Institute of India. The second one is Covaxin by Hyderabad based Bharat Biotech in collaboration with the Indian Council of Medical Research (ICMR)[11]. Usually, any vaccine comes to the market after all the three phases of their clinical trials are over, which takes a long period, typically in years. However, for the COVID-19 vaccines, the phases were accelerated. Phase 3 of the clinical trial of Covishield started in August, and the interim results were published in the Lancet. Evidence was reported that the vaccine could prevent COVID-19. The Covaxin, however, had received the nod of using it before phase 3 of the clinical trials were complete[12]. This has raised the eyebrows of some experts. However, favorable arguments exist as well. After the initial results of phase 3 trials, the green signal was given as it was believed that it would ultimately save more lives than cause damage in these unprecedented circumstances. After all, everything is fair in love and war.
Bibliography
Subhajit Bandyopadhyay, although a Professor of Chemistry, prefers to call himself a lifelong student. He loves to travel, and dabble with his paintbrushes. He is also associated with Cogito137 since its inception.
signup with your email to get the latest articles instantly